The scale of the data that healthcare businesses work with, and the complex data formats used, are just two of the many reasons why you need modern data platforms to effectively solve those complex data challenges.
CloverDX is a data platform that helps you automate your data workflows - eliminating manual steps, freeing up time and reducing errors. Because it's source and format agnostic, you can handle data from multiple sources (such as EHR systems, benefits administrators, insurers or many more), and work with often complex healthcare data formats (e.g. HL7 or X12) more easily.
In this blog, we’ll unwrap four use cases where CloverDX met the needs of a company in the healthcare or insurance sector.
Use case 1: Processing variable and high-volume clinical data
‘Be lenient in the data formats you accept. Be strict in the data formats you produce.’ - Postel’s robustness principle.
In this first example, our client works with large-scale healthcare data to make it actionable.
Their overall process to work with data is straightforward enough. They take HL7 messages, then transform it into a standard JSON format, and then load it into their analytic warehouse. However, variability in formats and versions, and the fact that mapping requires input from domain experts (who don’t necessarily have developer skills) meant they needed support.
To help them resolve this, we made some key changes to make it simpler for the domain specialists to provide input into the mapping.
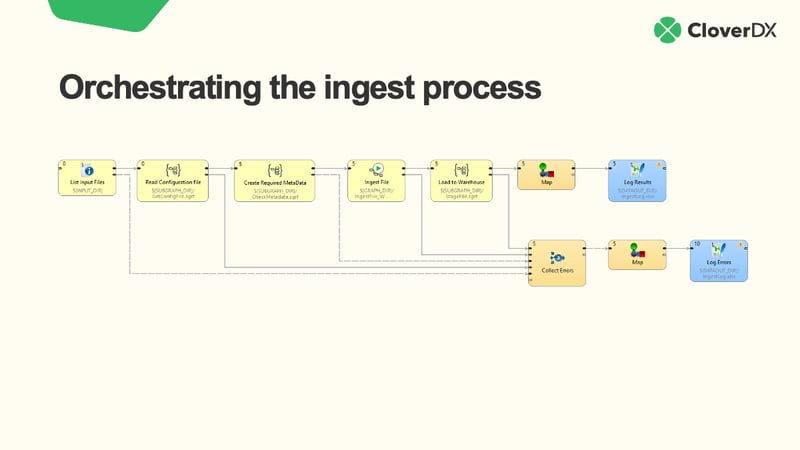
Watch a demo of the process in CloverDX:
First, we separated the mapping and transformation rules from the execution data pipeline itself. We then provided straightforward, easy-to-understand representations for expressing these rules using a format the domain experts were comfortable with (Excel in this example).
Here's a diagram to show what the mapping looked like:
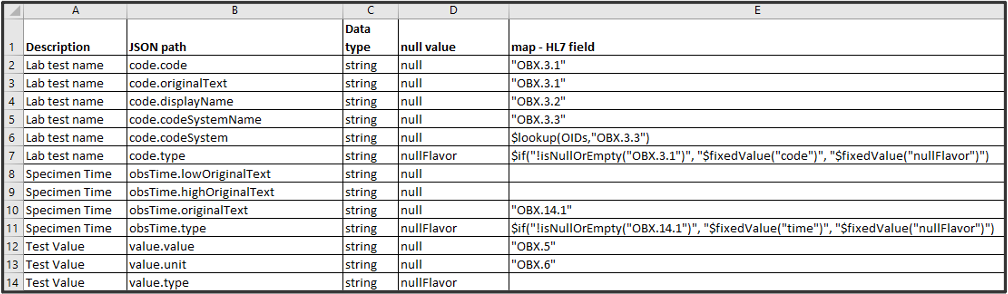
Once we have the mapping documents, we use these in the data pipeline. So, the HL7 data comes in, and then it’s translated to a ‘raw JSON’ format. Then, the mapping runs - grabbing the appropriate Excel doc, performing the required mapping, and creating a new JSON file that’s ready for processing and pushing downstream.
This method not only enables domain experts to provide inputs using tools they’re comfortable with but is also extensible. The pipeline can take any message, convert from any flavor of HL7, apply a custom mapping, and create an output file. What‘s more, it can run on autopilot, detecting new HL7 messages as they arrive and running the mapping automatically, so the clean JSON can go into the analytic warehouse.
Use case 2: Automating ingest of healthcare plan descriptions
In the US, health insurance providers offer many different plans. Our client helps simplify the process of employers choosing which plans to offer their staff by collecting and analyzing insurance plan descriptions for them. This helps employers get more control over both their costs and compliance.
The challenge our client faced was trying to automatically process these plans. The plans came as spreadsheets not well-optimized for a computer to read. And the plans would frequently change, for example, new columns, new rows, etc.
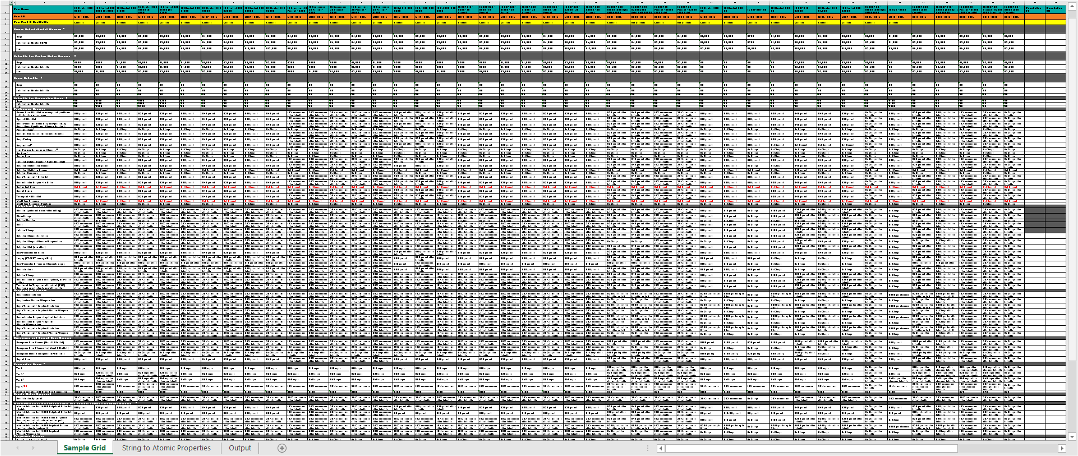
You can see how complex these spreadsheets can get:
Here's what our five-step automated solution looked like:
- Analyze the plan description spreadsheet to establish the structure
- Read the spreadsheet and extract the data
- Enrich with additional data
- Translate the plan description into JSON that’s fully qualified
- Upload the data to the warehouse
Now, our client can automate the process of extracting plan descriptions, so they can make accurate, up-to-date information available to their clients.
Watch a more in-depth explanation of this use case:
Use case 3: Automated processing of healthcare benefits enrollment
In this instance, our client manages the benefits enrollment activity for employers. Specifically, this means managing the process of people filling out forms to change their coverage. They act as an intermediary between health care consumers and the insurance provider.
Automating the data pipeline for our client here meant establishing a series of data enrollment events:
- Accept events in the form of EDI 834 formatted messages (the standard for healthcare benefits enrollment transactions).
- Validate the message format. If messages are invalid, return them for correction.
- Process messages if they are valid. This is done by comparing against current records and dispatching valid requests to the associated healthcare insurance company.
At the same time, there were automated audit reports of everything that happened. This means the customer can now see which reports are accepted or rejected, as well as what changes were made.
Thanks to the power of automation, our client can now handle more business without having to scale their headcount.
Watch the video for a walkthrough of this solution for automating the management of benefits change requests:
Use case 4: EHR data migration
In our fourth and final use case, we're looking at a client that provides integrated healthcare technology solutions to medical practices. This covers everything from practice management to managing EHR (Electronic Health Records) software. The challenge they brought on CloverDX for was migrating medical practices to a new EHR system.
Their business depends on the fast, economical and accurate onboarding of clients, moving them quickly and accurately from legacy EHR systems to our clients' platform.
To optimize these migrations, we helped template workflows for source EHR systems. This allowed existing staff to handle more data migrations whilst at the same time reducing errors. Of course, this also makes re-migrations faster if the initial migration exposes data issues that require a re-run.
In addition to these templated workflows, we created automatic audit reports. This improved customer confidence that the migration went well.
The final video clip describes how the architecture built with CloverDX worked to create faster, more efficient data migrations, and to enable the same process to be used for migrations from different systems.
Ready to solve 100% of your healthcare data challenges?
As we’ve seen, healthcare tech and insurance companies face a myriad of data challenges. Most healthcare data processing is complex, having to go beyond standard data formats.
But good data pipeline design - helped by flexible, customizable data tools like CloverDX - can help simplify the base solution, the common parts of moving data from A to B, allowing you to focus on the healthcare-specific tasks.
If you’d like to hear more about any of the solutions above, or see if CloverDX could help build a solution for your healthcare data process, just get in touch here and we'll get right back to you.